Plantar Fasciitis
 Plantar fasciitis is a condition describing heel pain over the tubercle of calcaneum where the plantar fascia inserts.
Plantar fasciitis is a condition describing heel pain over the tubercle of calcaneum where the plantar fascia inserts.
Definition:
Plantar fasciitis is a condition describing heel pain over the tubercle of calcaneum where the plantar fascia inserts. The term, fasciitis, is probably a misnomer because active inflammation of the plantar fascia is very rare.
Symptoms and signs:
Patients usually do not have symptoms of inflammation, such as night pain or rest pain. Most of the patient’s symptoms are mechanical with heel pain that interferes with normal walking. Pain is most severe when patient starts to walk after prolong resting, e.g. rises from bed or sofa. Women may find that pain is less severe when they wear high heel shoes. Generic sole pads or arch supports may ease the pain for a short time and usually does not help much permanently. Often patients give a history or unaccustomed long period of walking, jogging or standing.
Patient may walk in the consultation room with an antalgic gait. Examination shows localized tenderness and swelling without signs of acute inflammation (due to tendonosis) over tubercle of the calcaneum. Doriflexion of toes shows up the tight plantar fascia which may trigger off the pain. Some patient may have tenderness over the interosseous ligament and lateral ligaments of the ankle joint indicating that there is an unstable ankle. Some may have painful spring ligament or subluxed cuboid suggesting a collapsed longitudinal foot arch.
Cause and biomechanics considerations:
The cause of injured plantar fascia is prolonged excessive mechanical stress. When a patient has an unstable ankle or a collapsed longitudinal foot arch, the plantar fascia is strained by the increased distance between its attachments, namely metatarsal heads and tubercle of calcaneum, mainly due to the over-pronated feet. Repeated strain and stress will cause micro-tears and, with time, painful tendonosis will be resulted. Stress to plantar fascia is further aggregated if the patient has an unstable mid-tarsal joint and tight calf muscles. Detail foot and ankle biomechanical assessment is necessary to find out the root cause of this condition.
Clinical Stages:
There is no objective clinical staging of this condition. However, severity may be graded according to whether pain affects the daily routine of the patient or not. Walking pain may not be serious for a white-collar, who sits most of the time, but would be very serious for a waiter, who has to stand or walk the whole day.
Investigations:
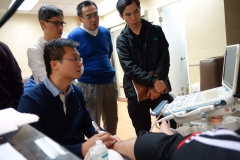
The diagnosis is mainly clinical. Musculoskeletal ultrasound may show bony spur and the classical features of tendinosis (thickened enthesis with hypoechoic lesions and underlying cortical irregularities, but without the firing on the colour flow mapping). Occasionally, ultrasound may pick up the associated tendon tears, ligaments injuries and soft tissue swelling. X-ray often shows calcaneum bony spur, which is the result of the injury to the enthesis but not the cause of the complaint. This is the most common myth and misnomer among the medical professions.
Treatment:
Treatment protocol often includes pain control, correction of biomechanical abnormalities, mobilization of tarsal bones, and therapeutic exercises. Cold padding helps to calm the heel pain at acute stage. When patient presents with severe pain, NSAIDs or even opioid analgesics may be required to alleviate the symptoms. After acute pain is controlled, it is wise to switch to simple analgesics, such as paracetamol, to avoid side-effects of NSAIDs. Intra-lesional corticosteroid is not recommended because of the inherent risk of tendon rupture with corticosteroid on weight bearing joints. Physiotherapists may offer shock-wave stimulation. Musculoskeletal physicians will focus on correcting biomechanical abnormalities and prevent recurrence. Prolotherapy is a very useful treatment modality to repair the tendonosis and associated ligaments injuries. Corrective orthotics is essential to support the collapsed foot arch if any.
足底筋膜炎
 足底筋膜炎指的是在足底筋膜接合跟骨結節附近出現的腳跟痛。"筋膜炎"這個名稱可能有點用詞不當,因為一般來說,足底筋膜是極少出現急性炎症的。
足底筋膜炎指的是在足底筋膜接合跟骨結節附近出現的腳跟痛。"筋膜炎"這個名稱可能有點用詞不當,因為一般來說,足底筋膜是極少出現急性炎症的。
定義:
足底筋膜炎指的是在足底筋膜接合跟骨結節附近出現的腳跟痛。"筋膜炎"這個名稱可能有點用詞不當,因為一般來說,足底筋膜是極少出現急性炎症的。
症狀與表徵:
病人一般不會出現發炎的症狀,例如在夜間或休息時感到疼痛。大多數病人的腳跟痛都是和力學有關,並影響了正常行走。疼痛通常在長時間休息後、再度走路時最嚴重,例如起床後或久坐沙發之後。女性可能會發現她們穿高跟鞋的時候,痛症會稍微減輕。一般的鞋墊或足弓墊可能可以在短期內舒緩痛楚,但長遠來說幫助不大。詢問病情時,病人往往表示曾試過長時間地非習慣性走路、跑步或站立。
病人在診室裡行走的時候可能會呈"減痛步態(antalgic gait)"。檢查結果顯示,跟骨結節附近出現局部壓痛和腫脹,但沒有急性發炎的表徵。背屈(Doriflexion)腳趾時會呈現過緊的足底筋膜,這可能是引起疼痛的原因。如果病人踝關節的骨間韌帶及外側韌帶出現壓痛,代表腳踝不穩定。如果病人足部的彈性韌帶異常疼痛,或骰骨出現半脫位,表示縱向足弓下陷。
病因及與生物力學的關系:
足底筋膜受傷的原因主要是長期承受力學上過度的壓力。當病人出現不穩定的腳踝或者縱向足弓下陷時,足底筋膜就其附著的蹠骨頭和跟骨結節之間的距離因足部外翻而變長和拉緊;重覆的拉緊及壓力會導致細微撕裂,久而久之,就會演變成肌腱退化(tendinosis),帶來痛楚。如果病人的中蹠關節不穩定以及小腿肌肉緊繃,足底筋膜的壓力就會更大。在這種情況下,需要進行詳細的足部及腳踝生物力學評估來找出根本原因。
臨床階段:
足底筋膜炎並沒有一個客觀的臨床階段。不過,此症的嚴重程度可以根據病人的日常生活如何受到疼痛的影響來進行分級。行走時的痛楚對白領人士的影響可能沒有那麼嚴重,因為他們大部分的時候都是坐著的;但對於經常要站立或走動的人士,例如侍應生來說,就可以說是嚴重地影響到日常生活了。
檢驗:
足底筋膜炎的診斷主要是臨床的。肌骼超聲波掃描可能會顯示出骨刺,以及典型的肌腱退化的特徵(著骨點增厚、出現低回音病變,骨表皮不規則,但彩色血流圖上沒呈火焰狀)。超聲波偶爾會檢測到相關的肌腱撕裂、韌帶損傷以及軟組織腫脹。足部X光通常可以顯示出跟骨骨刺。注意,跟骨骨刺一般是因為著骨點受傷而引起的,骨刺本身不是痛症的原因,這是醫學界普遍存在的誤解。
治療:
治療方案一般包括疼痛控制、糾正生物力學上出現的問題、跗骨舒展運動,以及治療性運動。冷敷有助於減輕急性的腳跟痛。如果病人出現嚴重的痛症,可能需要處方非類固醇類消炎劑(NSAIDs),甚至可待因類止痛劑來舒緩病情。不過當急性痛症得到控制之後,最好是換成普通的止痛劑,例如撲熱息痛,以避免非類固醇類消炎劑的副作用。不建議使用在患處注射類固醇(intra-lesional corticosteroid),因為有導致負重關節肌腱斷裂的潛在危險。物理治療師可能會應用震波刺激療法。肌骼科醫生則會集中於糾正生物力學上的問題以及預防疾病再度發生。保絡療法(prolotherapy)是修復肌腱退化及韌帶損傷很有效的治療方法。如果足弓下陷,則要配合矯正鞋墊。