Osteoarthritis of Knee
 Osteoarthritis of knee is a degenerative joint disorder of knee.
Osteoarthritis of knee is a degenerative joint disorder of knee.
Definition:
Osteoarthritis of knee is a degenerative joint disorder of knee. According to the America College of Rheumatology, diagnosis is made when a patient has knee pain and three of the following features – age over 50 years, stiffness less than 30 minutes, joint crepitus, bony enlargement, bony tenderness, and no palpable warmth. Osteoarthritis is a result of imbalance of cartilage synthesis and degradation, which causes fibrillation of cartilage surface and clustering of chondrocytes around fibrillation clefts. There is increase collagen and proteoglycans synthesis as well as degradation, causing rupture of collage network and osteophytes formation. When bone surface is exposed, synovial fluid can penetrate the small crevices, resulted in subchondral bone cyst.
Symptoms and signs:
Patient often presents with either unilateral or bilateral knee pain, which is associated with movements and relieved by rest. Occasionally, pain may come abruptly with sudden exacerbation of symptoms, which is an indication of acute flare-up. However, other causes like gouty arthritis, infectious arthritis or intra-articular loose body should be excluded. Knee swelling is not uncommon. Swelling may due to joint effusion, Baker’s cyst, bony swelling or hypertrophy of synovium.
Examination begins with observation. Patient may have lower limb deformity and walking with swaying side to side rather bending the knees. Genu varum deformity is often found in patient with advanced disease. There is usually no increase local warmth. Depending on the severity of the problem, range of movement may be limited. At end range of motion, severe arthritic changes may give a hard end feel while intra-articular loose body gives a springy end feel. Local tenderness is often present at femoral condyles, medial collateral ligament and pes anserine. Classical sign is the presence of crepitus on patellar grinding.
A musculoskeletal physician will pay attention to the effect of the disease on the patient’s activities of daily living as well as its impact on the psychosocial well-being. Over dependence on walking aids may lead to adaptation of abnormal walking pattern. Hyper-vigilance to pain may lead to pathological pain behaviors. Therefore, it is advisable to note down the severity of and pain and its associated problem in the clinical notes.
Cause and biomechanics considerations:
Osteoarthritis is often attributed to natural aging. Other risk factors include obesity, lack of exercise, female sex and repeated joint insults which include meniscectomy, previous inflammatory joint diseases, high impact sports, sport participation with abnormal joints and occupation that requires much knee bending and lifting e.g. heavy manual, mining and dockyard workers.
Abnormal lower limb biomechanics may increase strain and stress to the knee. Genu valgum or lock knee would increase stress to medial compartment. Over-pronating foot will cause tibia internal rotation during full foot bearing, which in turn lead to compensatory femoral internal rotation to unlock the knee and resulted in grinding of lateral femoral condyle on the undersurface of the patella. Female has a wider pelvis and have a larger Q angle, which also contributes to osteoarthritis.
Clinical Stages:
Osteoarthritis of knee may be classified according to X-ray changes.
Stage 1 No X-ray changes
Stage 2 Narrowed joint space
Stage 3 Presence of osteophytes
Stage 4 ‘bone on bone’ with very narrow joint space
WOMAC is another method of staging, which is based on symptoms and degree of disability and it is a good predictor of future surgery or knee replacement.
Investigations:
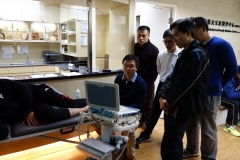
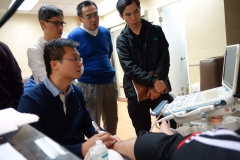
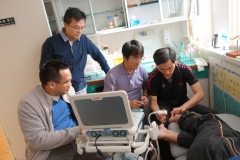
Osteoarthritis of knee is a clinical diagnosis. Imaging is not always necessary. Standing X-ray on AP view is useful for clinical staging. Sunrise view X-ray is indicated to exclude osteochondral loose bodies. Musculoskeletal physicians may use ultrasound imaging to document ligamental and tendinous injuries around the joint or the loss of cartilage at patellofemoral joint. Although peripheral meniscal tears may also be picked up during ultrasound imaging, MRI is indicated when there are clinical suspicions of meniscal tear or rupture of the cruciate ligaments.
Treatment:
Treatment depends on the presentation and severity of the injury. The aim is to control pain; strengthen muscles, improve balance and return to normal daily activities. Non-pharmaceutical modalities such as guided exercise, weight reduction, transcutaneous electrical nerve stimulation (TENS) may be useful to control the symptoms. Paracetamol, particularly the slow released formula in full dose, is useful to control mild to moderate pain. NSAIDs or COX2 anti-inflammatory drugs should be used when there is acute flare up of the condition. When there is co-morbidity or increased risks of using NSAIDs, tramadol or opioid analgesics should be considered. Dietary supplements, such as glucosamine, have contradictory evidences1 and users should consult their musculoskeletal physicians before taking these supplements.
Musculoskeletal physicians will formulate treatment plan according to the clinical needs of the patient. Intraarticular injection of Hyaluronan may provide temperate symptomatic relief. Prolotherapy is useful to restore damaged ligaments or tendons and stimulate cartilaginous regeneration and is particularly useful to patients with moderate severe osteoarthritis. For patient with end-stage osteoarthritis, knee joint replacement is probably the treatment choice.
References:
膝部骨關節炎
 膝骨關節炎是一種膝關節退化性疾病。
膝骨關節炎是一種膝關節退化性疾病。
定義:
膝骨關節炎是一種膝關節退化性疾病。根據美國風濕病學會的定義,如果出現膝痛,再加上以下至少三項症狀,就可以診斷為退化性膝關節炎:50歲以上、關節持續僵硬不超過30分鐘、活動時出現骨摩擦音(劈啪響聲)、骨頭發大、骨壓痛,以及摸不到膝關節有發熱的情況。骨關節炎一般是因為軟骨的合成和降解不平衡所引起的。軟骨的合成和降解不平衡會導致軟骨表面纖狀化,軟骨細胞並會在纖狀裂口處聚集。骨膠原和蛋白聚糖的合成及降解均會增加,造成膠原網絡的斷裂和骨刺的形成。當骨表面裸露出來,滑膜液就能從其小裂隙滲入,形成軟骨下骨囊腫。
症狀與表徵:
病人往往會有單則或雙則膝蓋疼痛的問題;痛症一般與病人日常的活動有關,可以通過休息來舒緩。有時,痛症會突然來襲,症狀也驟然惡化,這是急性發作的跡象。不過,診斷時應該排除其他病因,例如痛風關節炎、感染性關節炎,或關節內有小異物游走。膝關節腫脹並不少見,腫脹可能是因為積液、貝克氏囊腫 (Baker's cyst)、骨腫脹或滑膜變得肥厚而引起。
做檢查的第一步是觀察。病人的下肢可能會有畸形的情況,走路時可能會利用身體左右擺動替代膝蓋彎曲。嚴重膝骨關節炎的患者通常會出現膝內翻的變形。患者的膝部皮溫一般沒有升高。關節活動範圍的受限程度則視乎膝蓋問題的嚴重程度而定。在關節活動範圍的終點,檢查嚴重關節炎時會有一種堅硬的感覺,而檢查有小異物游走的關節時會有種回彈的感覺。檢查股骨髁、膝部內側副韌帶及鵝足肌一帶一般會有局部壓痛。最典型的表徵是髕骨(膝蓋)磨擦時會發出劈啪響聲。
肌骼科醫生會留意膝骨關節炎對病人日常生活、心理、社交方面的影響。如果過度依賴助行器步行可能會令病人習慣了不正確的行走模式。對疼痛過度反應可能會引致病理性的疼痛行為。因此,最好在臨床記錄中記下疼痛的嚴重程度以及疼痛引起的相關問題。
病因及與生物力學的關係:
骨關節炎通常是人體自然老化引起的。其他的高風險因素包括肥胖、缺少運動、女性,以及重複性關節損傷,例如半月板切除、曾患過發炎性的關節疾病、進行高衝擊性運動、關節異常時仍參加體育運動,以及需要膝蓋經常做出彎曲和起立的工作,如採礦、造船及需要大量體力勞動的工人。
下肢異常的生物力學可能會增加膝關節的壓力。膝外翻或膝關節交鎖 (lock knee) 會增加膝內側腔室的壓力。足部過度內翻會使脛骨在足部負重時出現內轉,股骨因而要作同樣內轉以鬆解膝部的扭力,此舉令膝蓋外走而令其底部與股骨外髁出現磨擦。此外,女性的骨盆及股四頭肌角 (Q angle) 較大是較易患上骨關節炎的原因之一。
臨床階段:
膝部骨關節炎的嚴重程度可以根據X光掃描的膝部病變來分級:
第一級 膝部沒有出現變化
第二級 關節間隙變窄
第三級 出現骨刺
第四級 "骨接骨"現象 – 關節間隙非常狹窄
WOMAC骨關節炎評分量表是膝骨關節炎分類的另一方法,它是通過評估患者的症狀及傷殘的程度來分級;WOMAC評分量表同時也是預測患者將來需要做手術或進行膝關節置換的一個有效指標。
檢驗:
膝骨關節炎的診斷主要是臨床的。放射性掃描並不是每次都需要。站立式X光的前後位圖像 (AP view) 對於臨床階段的分級很有用;日出位圖像 (sunrise view) 則可以掃描髕股關節。肌骼科醫生可能會用超聲波掃描來檢查關節周圍的韌帶和肌腱是否受傷,或髕骨關節的軟骨是否缺損。雖然超聲波掃描也可能檢測到半月板周邊的撕裂情況,但如果臨床有懷疑半月板撕裂或十字韌帶斷裂,則應該使用磁力共振掃描。
治療:
治療方案要視乎症狀及損傷的嚴重程度而定。治療的目的是控制痛症、強化肌肉、改善平衡力,及恢復日常的活動。非藥物療法,例如指導性運動、減肥以及透皮神經電刺激 (transcutaneous electrical nerve stimulation, TENS),對控制症狀可能會有用。扑熱息痛 (Paracetamol),特別是量緩釋配方,服用全劑量有效於控制輕微至中度的痛症。如果是急性發作,可以處方非類固醇類消炎劑 (NSAIDs) 或環加氧酶-2消炎劑 (COX 2 anti-inflammatory drugs)。如果有共發病 (co-morbidity) 或者當使用NSAIDs的風險提高的時候,可以考慮處方曲馬朵 (Tramadol) 或阿片類鎮痛藥 (Opioid analgesics)。膳食補充劑,如服用葡萄糖胺效果的數據參差1,因此病人在服食這些補充劑前應先諮詢肌骼科醫生的意見。
肌骼科醫生會根據個別病人的臨床需要而定出治療方案。透明質酸 (Hyaluronan) 的關節注射可以短暫地舒緩症狀。保絡治療 (Prolotherapy) 在恢復損傷的韌帶或肌腱、及刺激軟骨更生方面療效顯著,特別是患上中度至嚴重骨關節炎的病者。對於晚期的膝骨關節炎患者來說,膝關節置換術可能是最佳的治療選擇。
參考文獻: