De Quervain Tenosynovitis
 Fritz de Quervain is a Swiss surgeon who published a case report of 5 patients with thickened first dorsal compartment of wrist more than 100 years ago and therefore the name “De Quervain syndrome”.
Fritz de Quervain is a Swiss surgeon who published a case report of 5 patients with thickened first dorsal compartment of wrist more than 100 years ago and therefore the name “De Quervain syndrome”.
Definition:
Fritz de Quervain is a Swiss surgeon who published a case report of 5 patients with thickened first dorsal compartment of wrist more than 100 years ago and therefore the name “De Quervain syndrome”. De Quervain tenosynovitis is the inflammation of the tendons in the first compartment of the dorsal wrist (the abductor pollicis longus [APL] and the extensor pollicis brevis [EPB] muscles), which become tender, swollen and cause entrapment under the tendon sheaths.
Symptoms and signs:
The symptoms of De Quervain tenosynovitis is basically pain. Patients usually give a typical history of pain over the radial side of the wrist with thumb or wrist movements. Because the APL and EPB tendons are inflamed and swollen, patients may complain about a tender swelling over the radial styloid region of the wrist. Redness over that area may also be seen in some cases. Triggering of wrist or thumb movement is rarely noted by patient.
On inspection, the first dorsal compartment of wrist joint is swollen and thickened over the radial styloid area. Erythema and increased skin temperature may be found if there is acute inflammation. Tenderness can be elicited over the inflamed and thickened tendons on palpation.
Special tests can be performed to diagnose this condition. Finkelstein test is performed by grasping the patient’s thumb and hand and ulnar deviating them together sharply. A modified Finkelstein test called Eichoff test, is performed by ulnar deviating patient’s fist which is made by the thumb flexed into centre of palm and then grasped by the fingers. In De Quervain syndrome, both tests will reproduce patient’s pain. As both tests are very painful, the ulnar deviation should be done very gently.
Common causes:
The exact cause of De Quervain tenosynovitis is not known. It may be a repetitive stress injury (RSI) caused by repetitive wrist movements in the coronal plane. Such repetitive movements are commonly found in mothers taking care of newborn babies, office workers using the computer mouse and people thumb typing on handheld devices. Therefore, De Quervain syndrome is commonly called by patients as “mother’s thumb” and even “blackberry’s thumb”. Apart from RSI, the APL and EPB tendons may be injured by acute sprain or strain at work or during exercise leading to De Quervain tenosynovitis. Patients with diabetes and autoimmune diseases, like rheumatoid arthritis, are at increase risk of developing De Quervain tenosynovitis.
Biomechanics considerations:
The APL and EPB tendons are required to raise the thumb up. These two tendons are tightly bound in the first dorsal wrist compartment over the radial styloid process by the overlying extensor retinaculum. Any swelling, edema or thickening of the tendons will hamper the gliding movement of the tendons in the already tight compartment causing pain and restriction of thumb abduction and extension at the wrist joint. To compensate for this, De Quervain patient often hyper-extends the thumb at the metacarpo-phalangeal joint (MCPJ) during thumb extension.
Investigations:
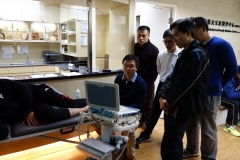
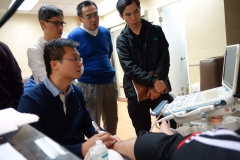
History and physical examinations are good enough to diagnose De Quervain syndrome. However, if fracture is suspected, X-ray is indicated. Musculoskeletal ultrasound is useful in visualizing the injured part of the tendons which is thickened and hypoechoeic. Sometimes, the APL and EPB tendon can have its own independent compartment in the wrist and this variation can be seen under musculoskeletal ultrasound. Such finding is important for treatment as blind injection may deposit the injectable into only one of the 2 compartments leading to treatment failure. In chronic De Quervain syndrome, the APL and EBP may be seen under ultrasound imaging to fuse together to form a swollen structure in the compartment. Also the color flow mapping tool of the ultrasound machine can provide additional information on severity of the tendon inflammation.
Treatments:
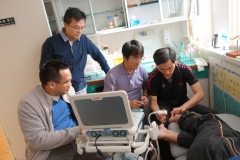
During the acute phrase, ice pack is used to release the inflamed symptoms. Splinting with thumb spica is effective in immobilizing the thumb to provide rest for the inflamed tendons. Pharmacological treatments with oral or topical non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used to relieve the pain and inflammation of the tendons. Steroid injection is a highly effective treatment modality for De Quervain syndrome1. For those who do not want steroid injections, prolotherapy under ultrasound guidance is also very effective. Non-pharmacological treatments by physical therapy and occupational therapy are important in correcting the dysfunctioning biomechanics and prevent relapses. If all these treatments fail, surgical release of the first dorsal compartment can be performed to release the tendons entrapment.
Reference:
狄魁文氏腱鞘炎
 奎爾狄魁文氏(Fritz de Quervain)是一位瑞士外科醫生,他在100多年前發表了一份關於五位病人手腕第一背腔室增厚的病例報告,這種腱鞘炎(tenosynovitis)自此就稱為“狄魁文氏症”。
奎爾狄魁文氏(Fritz de Quervain)是一位瑞士外科醫生,他在100多年前發表了一份關於五位病人手腕第一背腔室增厚的病例報告,這種腱鞘炎(tenosynovitis)自此就稱為“狄魁文氏症”。
定義:
奎爾狄魁文氏(Fritz de Quervain)是一位瑞士外科醫生,他在100多年前發表了一份關於五位病人手腕第一背腔室增厚的病例報告,這種腱鞘炎(tenosynovitis)自此就稱為“狄魁文氏症”。狄魁文氏症指的是手腕背的第一腔室的肌腱(外展拇指長肌及伸拇指短肌)因為發炎而出現壓痛、腫脹,因而在鞘膜內受到卡壓。
症狀與表徵:
此症的症狀基本上就是疼痛。病人通常有典型的手腕側疼痛的病史 ------ 拇指或手腕活動時手腕橈側會感到疼痛。由於外展拇指長肌及伸拇指短肌發炎並腫脹,病人可能會抱怨手腕的橈骨莖突附近出現壓痛及腫脹;某些病人的患處可能還會發紅。不過病人一般很少注意到手腕或拇指伸展時會有彈跳 (triggering)。
檢查病人的腕關節時,可以在橈骨莖突附近發現腫脹及肥厚的第一背腔室。如果是急性炎症的話,可能還會檢查到紅斑,病人的皮溫也會上升。觸診發炎及變厚的肌腱時會產生壓痛感。
特別的理學檢查可幫助診斷。典型的測試是“芬克爾斯坦測試(Finkelstein test)”,即握住病人的拇指和手掌,然後把它們急速一齊作尺向偏移。另外一個改進的芬克爾斯坦測試是Eichoff test,即把拇指內收於手掌內,再用其他四指握拳把它包住,然後作尺向偏移。如果病人患上狄魁文氏症,兩種試驗均會引起痛楚。也因為兩種試驗都會帶來痛楚,所以進行尺向偏移時動作要較為緩慢及小心。
常見的原因:
引起狄魁文氏症的原因暫時還不清楚,它可能是手腕經常在冠狀切面重複某些動作、而引起重複性施壓損傷(repetitive stress injury, RSI)有關。這種重複性的動作常見於剛生產過後照顧BB之婦女、長期使用電腦滑鼠的上班族,以及經常以拇指在手機打字的人士。所以,病人普遍把狄魁文氏症稱為“媽媽手”,甚至“黑莓手機手”。除了重複性施壓損傷(RSI)外,病人也可能在工作或者做運動的時候發生急性扭傷或拉緊,而令外展拇指長肌及伸拇指短肌受傷,繼而引起狄魁文氏症。糖尿病及自身免疫病的患者,例如類風濕性關節炎,則是狄魁文氏症的高危一族。
與生物力學的關係:
我們平時需要外展拇指長肌及伸拇指短肌來豎起大拇指,這兩條肌腱緊緊地縛於手腕的第一背腔室內,上有伸肌支持帶(extensor retinaculum)遮蓋,下面則是橈骨莖突部,兩條肌腱被約束在這個本來就狹窄的鞘管內,任何的腫脹、水腫或增厚都會進一步限制了它們在腔室內的滑動,引起痛症;並限制了大拇指在腕關節的外展和伸展動作。因為這樣,病人在伸展大拇指的時候往往需要大拇指的掌指關節(metacarpo-phalangeal,MCP)以超正常的伸展作補償。
檢驗:
了解病史及身體檢查已足以診斷出狄魁文氏症。但如果懷疑有骨折,就應該照X光。肌骼超聲波掃描可以清楚顯示出受傷的肌腱部位(變厚及出現低回音病變)。有時,外展拇指長肌及伸拇指短肌在手腕處可能會有自己的腔室,肌骼超聲波掃描亦可以檢測出這種變異。此檢驗結果對注射治療是否成功有很重要的作用,因為盲目注射可能會使藥物只注射到兩個腔室中的其中一個,最後引致治療失敗。在慢性的狄魁文氏症,肌骼超聲波掃描見到的外展拇指長肌及伸拇指短肌可能已經融合在一起,在腔室內形成一個腫大的組織。而超聲波掃描器內的彩色血流圖(color flow mapping)功能還可以提供肌腱發炎的嚴重程度資料。
治療:
在急性期,冰敷有助於減輕發炎的症狀。另外,可以用拇指人字型夾板(thumb spica splint)來固定大拇指,讓發炎的肌腱休息一下。藥物治療方面,常用的包括口服或局部的非類固醇類消炎劑(NSAIDs),可以舒緩痛症及炎症。類固醇注射是醫治狄魁文氏症一種很有效的方法1;如果不想接受類固醇注射,在超聲波引導下進行保絡治療(prolotherapy)的效果也很好。非藥物治療方面,物理及職業治療可以有效糾正生物力學上出現的問題,以及預防病情復發。如果這些治療方案都起不了作用的話,可以考慮進行手術來鬆解被卡壓的肌腱。
參考文獻: